|
Treatments during the early 20th century
Read a descriptive text by Lena Carlsson, and learn about a reality only two generations back in time.
The photographs above belongs to the "Medicinhistoriska Museet" in Lund, Sweden.
A lot has happened since the beginning of the 20th century. A hundred years ago, the mentally ill were treated in asylums. Many of the treatments used during these days appear frightening to people today. It is however important to remember that the doctors had a very difficult task, and were desperately looking for methods and treatments to help the ill.
 The picture shows a plant of Datura metel. A double yellow specimen is depicted.
The picture shows a plant of Datura metel. A double yellow specimen is depicted.
In the beginning of the twentieth century when Ester Henning and her sister Rut became ill there neither existed any known efficacious therapies against schizophrenia, nor against any other psychical diseases. Ancient but inactive methods like bleeding, emetics and purgatives from the age of Hippocrate in the fifth century before Christ survived for a long time here and there, but they more and more disappeared during the nineteenth century. Other substances with a long history are alcohol and opium which were used as comforting and sleeping medicines. So did alkaloids from the vegetable kingdom, such as scopolamine and atropine from the plants thorn apple, belladonna, henbane and mandrake. In high doses the alkaloids can provoke psychotic-like states. Maybe it was therefore one believed that lower doses could cure madness.
Calming and soporific effect of chloral hydrate
In 1869 the doctors began to utilize chloral hydrate, which has a calming and soporific effect and sometimes replaced opium. Chloral hydrate reduced anxiety in psychotic persons and helped them to sleep. This medicine brought a calmer atmosphere to the asylums. In 1903 the barbiturates made their entrance. They were safer and more efficacious soporifics and sedatives than chloral hydrate. But the sleeping-draughts are addictive and they have other negative effects as well. Neither can they eliminate hallucinations and other psychotic symptoms.
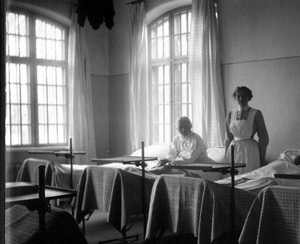
During the time period, 66 years, that Ester Henning spent at various asylums, many things happened within Swedish mental health services. In the first years of her illness Ester Henning often lay in bed. Confinement in bed, which was introduced in the end of the nineteenth century, was a frequently used method to keep the patients calm. Psychical diseases were regarded as physical diseases that affected the brain. The bedridden state was supposed to give rest, protect against impressions and facilitate the blood circulation of the brain. Moreover, the patients became easier to superintend and they were prevented from making trouble. When confinement in bed was brought out the small single cells at the asylums were rebuilt to large halls with up to 40 patients in each, to save the personnel.
 Strait-jackets and other means of compulsion
Strait-jackets and other means of compulsion
At the new asylums the idea was to utilize as few means of compulsion as possible. This was also made easier by the confinement in bed. Nevertheless, sometimes various means of compulsion had to be resorted to such as strait-jackets, shoes with locks, dresses that were locked at the bottom, and gloves that were tied around the wrists to prevent the patients from tearing themselves. The strait-jacket, however, seems to have been used seldom since the end of the nineteenth century.
 The picture belongs to the Medicinhistoriska Museet, Lund. Click on the picture to see a larger photography.
The picture belongs to the Medicinhistoriska Museet, Lund. Click on the picture to see a larger photography.
Bathing therapy lasting for days
During the later part of the nineteenth century bathing therapy was introduced. Even the bathing therapy which was utilized right up to the end of the nineteen forties, aimed at calming the anxious patients. The patient was submerged into a water of 36 degrees Celsius, and sometimes a sail with a hole for the head was fastened over him or her. The bathing lasted for a couple of hours or days. Some individuals probably had a comfortable and relaxed time, while others found it tough. The staff regarded the supervision of the bathing patients as the most trying of all the tasks at the asylum. These patients were not always so calm and easy to handle. They would scream and spatter so that water with excrement splashed over the attendant, who was often alone with up to five patients.
The story of Svea: "My skin fell off and the flesh appeared"
This is the story of Svea, in a book about mental hospitals and the history of psychiatry, written by the Swedish journalist Vanna Beckman. Svea lay in the bath day and night for three weeks:
| "My skin fell off so the flesh appeared, my feet became quite spongy and wrinkled. My hole body ached. They came and fed us there in the bath. Sometimes they gave me injections. I remember getting apomorphine because I kept singing so much. I sang ( a popular Swedish song about a seaman who loves the sea) during the round. The doctor then prescribed an injection. My head was in a whirl and I vomited. But then I was feeling better and I got going with my singing again. I beat time in the tub so that everyone should hear. The more they maltreated me, the worse I got."" |
Apomorfine and sleeping cures
Apomorpine which the doctor gave Svea provokes vomiting and was ordinated as a sedative. In the latest decades the American scientist Carol Tamminga has shown that apomorpine really has the ability to alleviate some psychotic symptoms. Other methods that were utilized in the beginning of the twentieth century were sleeping cures, where the patients got bromides or barbiturates which put them to sleep. In rare cases the sleeping cures lasted for several days, sometimes even weeks, with interrupts for feeding and personal care only.
Fever therapies did not help the schizophrenic patients In the nineteen thirties a number of new treatments were introduced into psychiatry. One of them was fever therapy, which became the first real cure against a mental illness. Since antiquity physicians had noticed that mad persons often ameliorated after a fever disease. The Austrian neurologist Julius Wagner von Jauregg discovered that malaria infection could improve the largest group among the mentally ill, that is those who suffered from paralysie gnrale (general paralysis of the insane). Sometimes as many as one third of the patients at the asylums had got that diagnosis. Paralysie gnrale is a brain disease with psychotic symptoms that arises in late stages of syphilis. von Jauregg received the Nobel prize in 1927 for his discovery. All kinds of fever therapies became popular at the mental hospitals, but they did not help the schizophrenic patients. However, the hope of also finding a cure against schizophrenia increased.
In the nineteen thirties a number of new treatments were introduced into psychiatry. One of them was fever therapy, which became the first real cure against a mental illness. Since antiquity physicians had noticed that mad persons often ameliorated after a fever disease. The Austrian neurologist Julius Wagner von Jauregg discovered that malaria infection could improve the largest group among the mentally ill, that is those who suffered from paralysie gnrale (general paralysis of the insane). Sometimes as many as one third of the patients at the asylums had got that diagnosis. Paralysie gnrale is a brain disease with psychotic symptoms that arises in late stages of syphilis. von Jauregg received the Nobel prize in 1927 for his discovery. All kinds of fever therapies became popular at the mental hospitals, but they did not help the schizophrenic patients. However, the hope of also finding a cure against schizophrenia increased.
New treatments launched in the middle of the nineteen thirties
At the middle of the nineteen thirties, though, pessimism once again began to spread within psychiatric care. Then two new treatments were launched - convulsion therapy and insulin. An optimistic attitude returned. The Hungarian doctor Ladislav von Meduna gave schizophrenic patients injections with camphorated oil, and later cardiazol, which provoke seizures. He reported on good results. The method was founded on the observation that schizophrenia and epilepsy seldom occur together, and when they do the psychotic symptoms usually decrease after an epileptic attack
The cramps were painful and risky
But the results were doubtful and the treatment was painful. The patient got an injection of cardiazol, which triggered between 15 and 30 attacks of cramps. The treatment was given twice a week during many weeks. Before curare came into use in 1957 it sometimes happened that older patients were stricken with fractures of the vertebrae. (Curare is a muscle relaxant.) Moreover, the cramps could be dangerous to the heart. Another great disadvantage was that the patients often experienced a strong anxiety after the injections with cardiazol. The cardiazol therapy was therefore soon weeded out among the methods of treatment.
 Simultaneously with cardiazol, insulin therapy was introduced. It was discovered when the Austrian psychiatrist Manfred Sakel tried to detoxicate drug addicts with insulin. By mistake he gave a too big dose of insulin, so the drug addicts landed up in coma, that is unconsciousness. The result was that the drug and its psychical effects disappeared more quickly. Therefore Sakel tested the treatment even on schizophrenic patients with good results. The patients who ameliorated often became ill again, though. Eventually, the doctors came to the conclusion that the positive effect that sometimes was seen probably resulted from the more careful nursing which the patients received at the special insulin wards. To be successful it was also important that the treatment was given to the patients during their first year of symptoms.
Simultaneously with cardiazol, insulin therapy was introduced. It was discovered when the Austrian psychiatrist Manfred Sakel tried to detoxicate drug addicts with insulin. By mistake he gave a too big dose of insulin, so the drug addicts landed up in coma, that is unconsciousness. The result was that the drug and its psychical effects disappeared more quickly. Therefore Sakel tested the treatment even on schizophrenic patients with good results. The patients who ameliorated often became ill again, though. Eventually, the doctors came to the conclusion that the positive effect that sometimes was seen probably resulted from the more careful nursing which the patients received at the special insulin wards. To be successful it was also important that the treatment was given to the patients during their first year of symptoms.
Ester Henning was spared both cardiazol injections and insulin therapy. Instead she was treated with electroconvulsive therapy, that is ECT, a new shock treatment that came into use in the end of the nineteen thirties. This treatment implies that current impulses are transmitted through the head, which leads to convulsions. ECT was introduced by the Italians Ugo Cerletti and Lucio Bini, who first provoked cramps with electricity in dogs, before any trials on humans were started. At the beginning sensational effects were seen, where patients who previously talked unintelligibly suddenly could be understood. ECT was considerably less risky than cardiazol and did not give rise to the same strong feelings of discomfort in the patients. ECT has also survived as a therapy and has shown good effect in depressions above all. Nowadays, however, the treatment is always given under narcosis and, since 50 years, with muscle relaxants so that no convulsions arise.
The method was quickly widely spread from the end of the nineteen thirties The most notorious of the methods of treatment in the previous century is perhaps lobotomy, where nerve fibers from the frontal lobe to deeper brain regions, which are locations for our emotional life, are cut off. The idea was that among other things anxiety and uneasiness should thereby diminish. Lobotomy was developed by the Portuguese doctor Egas Moniz who was awarded the Nobel prize in 1949 for his work. But the results of the operations were not very satisfactory. Many patients were surely less anxious and aggressive, but they also became indifferent and blunt. Despite of these circumstances, the method was quickly widely spread from the end of the nineteen thirties, because of Moniz' great authority and because many patients could be discharged. The surgeons began to test various kinds of techniques. The American neurologist Walter Freeman invented a rough method where he placed an ice-pick in the upper part of the eye, after having anaesthetized his patient. Then he knocked on the ice-pick with a hammer until it had penetrated five centimeters into the brain.
The most notorious of the methods of treatment in the previous century is perhaps lobotomy, where nerve fibers from the frontal lobe to deeper brain regions, which are locations for our emotional life, are cut off. The idea was that among other things anxiety and uneasiness should thereby diminish. Lobotomy was developed by the Portuguese doctor Egas Moniz who was awarded the Nobel prize in 1949 for his work. But the results of the operations were not very satisfactory. Many patients were surely less anxious and aggressive, but they also became indifferent and blunt. Despite of these circumstances, the method was quickly widely spread from the end of the nineteen thirties, because of Moniz' great authority and because many patients could be discharged. The surgeons began to test various kinds of techniques. The American neurologist Walter Freeman invented a rough method where he placed an ice-pick in the upper part of the eye, after having anaesthetized his patient. Then he knocked on the ice-pick with a hammer until it had penetrated five centimeters into the brain.
Many patients died or suffered from severe injuries
Together with the neurosurgeon James Watts, Freeman traveled around and marketed his surgical technique at the mental hospitals in the USA, by for instance making free operations in front of the staff and the journalists. After many years of lobotomy, however, the criticism increased. The method was badly evaluated and many patients died or contracted infections and epilepsy. Autopsies revealed extensive brain damages in the treated patients. One of those who died after a lobotomy was the Swedish artist Sigrid Hjertn, who was operated in 1948 at Beckomberga and died in a postoperative bleeding. Also the American film star and left-wing rebel Frances Farmer was treated with Freeman's knife.![]() Read more about Sigrid Hjertén
Read more about Sigrid Hjertén
Thousands of patients were lobotomized
During the nineteen forties and fifties more than 9000 persons were lobotomized in the Scandinavian countries, which belonged to the countries that performed the largest number of operations in relation to the population. In the USA the number of lobotomized patients was more than 40 000 in the same period. After the introduction of the new antipsychotic drugs in the beginning of the nineteen fifties the lobotomies were gradually heavily reduced. Still today, however, a minority of patients are operated in the brain every year in Sweden, to mitigate severe states of anxiety, where no other methods have helped. The operation which is called stereotactic capsulotomy is more exact today, and it is never executed against the patient's will.
 The picture shows the plant Rauwolfia serpentina.
The picture shows the plant Rauwolfia serpentina.
The greatest revolution within psychiatric care took place when a new efficacious drug against psychosis was synthesized, at the same time as an old Indian nature-cure medicine was rediscovered. In India the pulverized roots from the bush Rauwolfia serpentina have been utilized as a drug for a few thousands of years. Gradually Indian doctors discovered that this plant was especially active against psychotic anxiety and hypertension. In the sixteenth century the German botanist and doctor Leonard Rauwolf brought the medicine to Europe. There it was utilized to a varying degree but was forgotten in the end of the nineteenth century. Not until well into the twentieth century the Indian doctors succeeds in making Western scientist interested in the medical plant, because of its capability to reduce hypertension. In 1952 Swiss researchers analyze the roots and discover that the active substance is reserpine. When the doctors began to utilize reserpine against hypertension they found that this substance had a good effect in psychotic patients. The patients became calmer and started to function socially again. Unfortunately, though, some of them became depressed.
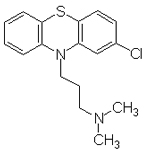 Illustration of the structure formula for chlorpromazine
Illustration of the structure formula for chlorpromazine
In the same year as reserpine was discovered, chlorpromazine was introduced. Chlorpromazine had similar mitigating effects in psychotic symptoms as reserpine. It was developed when French doctors were looking for quite another effect, a substance that could counteract deleterious reactions of the body when it is exposed to severe strain, for example a big operation or an accident with extensive physical injury. By reducing body temperature the doctors thought that the injuries could be reduced. They therefore searched for an antipyretic substance and finally found chlorpromazine. Since even persons with mental illnesses such as acute psychoses sometimes get high fever the substance was tested also in those patients. The French doctors Jean Delay and Pierre Deniker at the hospital of Saint Anne in Paris gave chlorpromazine to patients with hallucinations and thought disturbances, with good results. The patients became more relaxed and the psychotic symptoms were reduced. At the same time they were described as "indifferent", an effect which was then regarded as positive. In the nineteen fifties lithium which is efficacious against manic-depressive illness, was also introduced. Two other new groups of drugs that made their entrance in this period are the tricyclics which counteract depressions, and the benzodiazepines which are tranquilizing agents.
Also chlorpromazine has serious side-effects
It turned out that chlorpromazine was superior to reserpine, which often gave rise to depressions. However, also chlorpromazine has many serious side-effects, among others the above-mentioned indifference. Patients who are not acutely psychotic are easily too subdued by the medicine and lose their vitality. Moreover, there are a number of other negative effects that may be painful. In the beginning almost all patients at the mental hospitals received chlorpromazine, which was heavily overused. The doses were high but were gradually reduced. Today this drug is utilized in a far more restricted way, and the aim is to give the lowest possible dose.
 In his book about the history of psychiatry Tord Ajanki tells about a schizophrenic patient who is treated with chlorpromazine. The patient who is called Bengt has been active as a preecher. Bengt is taken to an asylum because of religious obsession and a nervous breakdown in 1943. At first he works in the bookbindery of the asylum, but later he changes for the worse and gets into a stupor during long periods, when he must be fed with a tube. Stupor, which may be a life-threatening state, implies that a person is quite immobile and remains in the position in which he is left. Drafts from the case-book also reveals that Bengt suffers a lot from feelings of guilt. He fights against voices that forbid him to eat, and he sees blood and corpses of women in the food. Bengt is also aggressive sometimes and it happens that he eats his excrements.
In his book about the history of psychiatry Tord Ajanki tells about a schizophrenic patient who is treated with chlorpromazine. The patient who is called Bengt has been active as a preecher. Bengt is taken to an asylum because of religious obsession and a nervous breakdown in 1943. At first he works in the bookbindery of the asylum, but later he changes for the worse and gets into a stupor during long periods, when he must be fed with a tube. Stupor, which may be a life-threatening state, implies that a person is quite immobile and remains in the position in which he is left. Drafts from the case-book also reveals that Bengt suffers a lot from feelings of guilt. He fights against voices that forbid him to eat, and he sees blood and corpses of women in the food. Bengt is also aggressive sometimes and it happens that he eats his excrements.
In the beginning of 1956, after many years of disease, Bengt gets chlorpromazine. One month later Bengt has stopped eating his excrements, he has started to weave and he behaves politely. In the summer Bengt gets permission to move freely about within the area of the asylum. After still many years of stay at the mental hospital Bengt is discharged. However, he never recovers completely, perhaps because chlorpromazine was given too him in such a late stage of his disease
Ajanki, Tor
Vanvettets kurer - om schizofreni.
Apotekarsocieteten 1999
Beckman, Vanna
Sinnessjukhuset. Bilder ur psykiatrins historia.
Publisher: PA Norstedt & Söners Förlag 1984
Bergström, Irja
"Ensam fågel - jag vet vem det är".
Ester Henning. Konstnärinna på hospital.
Gothenburg 1989
The dissertation is also available in a version for the general public, published at the Carlsson Förlag in 2001.
Harding, Gösta
Tidig svensk psykiatri.
Verbum 1975
Ljungberg, Lennart
Psykiatri ur ett Stockholmsperspektiv - en kort historik.
Ur Stockholms läkarförening 100 år. Sid 105-110.
Supplement till Läkartidningen 2000
Modern svensk sinnessjukvård.
Den psykiska sjukvården i Sverige förr och nu.
Redigerad av Gunnar Lundquist.
AB Modern Litteratur, Stockholm 1949
Tips on more websites with information in this area![]() Website with information about St Lars
Website with information about St Lars![]() Database on medical history
Database on medical history
By Lena Carlsson,
| Home |